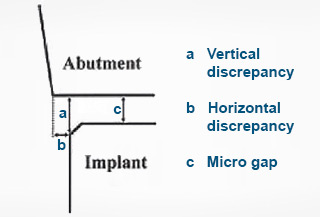
A Perspective on Microgaps
Are Microgaps a clinical problem?
There are, to our knowledge, no conclusive studies that correlate large microgaps with mucositus or peri-implantitis. There is also only low level evidence that large microgaps lead to greater bone loss around implants.
In spite of this, it has been the belief and passion of Southern Implants, to have minimal microgaps. We are probably the only manufacturer that does not deburr components by tumbling. Tumbling leads to a “V” shaped microgap at the interface. The second thing we do, is a microgap test of every single interfacing item that we make. This test identifies any component with a microgap greater than 1.5 microns, which is then subsequently rejected.
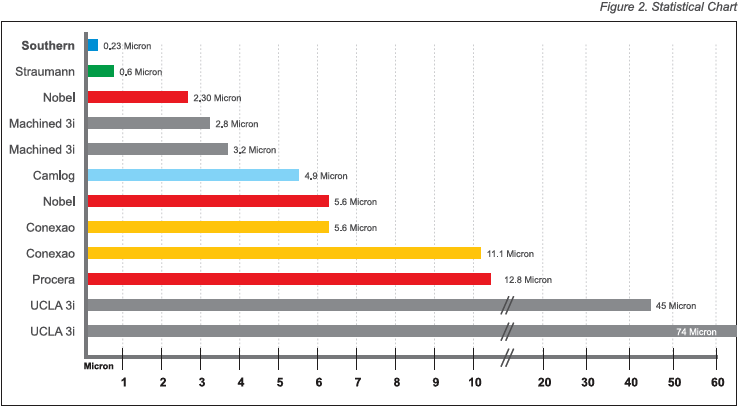
Most manufacturers have microgaps of 2-6 microns (Tsuge et al) whereas the Southern typical microgap is 0.23 microns (Dellow et al).
In a ten-year prospective clinical study of Southern Implants External Hex Implants, no patient has developed peri-implantitis and there has been no change in bone levels in the 5-10 year period.
In the extensive Cochrane Collaboration Review of March 2005, Esposito et al studied implant failure rates, rates of peri-implantitis and marginal bone response. They found that there was good clinical research data for only 4 systems (Astra, NobelBiocare, Southern and Straumann). No system had a better or worse rate of peri-implantitis.
A far greater concern is residual cement in cemented protocols. Residual cement is directly correlated to mucositis and bone loss. Hence the need to use screw retained protocols, especially in patients susceptible to peri-implantitis. Some connection types, especially deep conical, make screw retained protocols extremely difficult to achieve. One advantage of the Co-axis implant is to facilitate screw retention in almost all situations. This is a significant factor in preventing cement-induced mucositis and peri-implantitis.
Relevant Statistics |
||||||||||||||||||||||||||||||||||||
|
The smallest bacteria in the mouth measures 0.5 x 1.2 microns. But, these bacteria usually group together and a 2 micron filter usually eliminates all bacteria.
|
||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||
Why do External Hex Implants have an association with big microgaps? |
||||||||||||||||||||||||||||||||||||
|
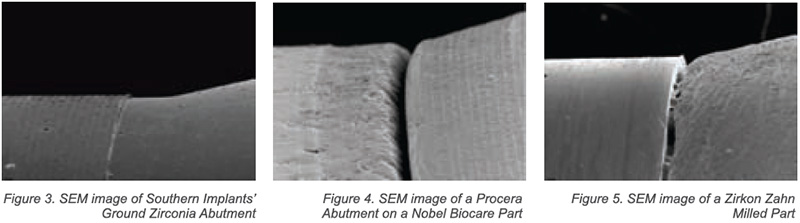
It all started when Dr’s Lewis and Beumer developed the UCLA Abutment as a burn-out plastic abutment, which is processed to become a casting direct to implant head. The investment casting process, no matter how skilled the technician may think that he is, will result in microgaps of at least 20 microns, and often up to 70 microns! Southern and 3i realized this to be sub-optimal and developed milling tools so that after casting, the seating surface can be “ground” with grinding paste and hence reduce this microgap to the desired 2 micron range. Sadly, few technicians are prepared to spend time to refine this surface. Secondly, the laboratories do not have the required equipment to make judgement on whether or not they have refined the surface adequately. The other approach that came about, was to use a cast-on gold cylinder which is machined, and when sold to the laboratory can have microgaps in the sub 2 micron range. However, the laboratory procedure subjects these parts to investing, devesting, and thermal cycling. Following these laboratory procedures, the microgap is usually above 10 microns and often as big as 40 microns. 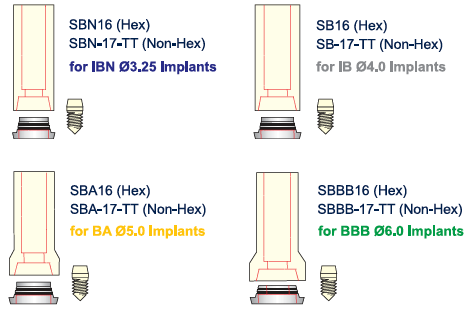
This lead to the development of the passive abutment, in collaboration with Dr. Andrew Ackermann. The titanium ring of this system is not subjected to the thermal cycling and is joined to the casting specifically to eliminate the microgap problem of laboratory-fabricated prostheses. So with the passive abutment a prosthesis can be made to fit direct to implant with a sub 2 micron microgap. If one fits an abutment (e.g. compact conical) to the implant, the microgap at implant interface is immediately controlled to be that of the manufacturers attention to detail, which in the case of Southern will be in the 0.23 micron range while other manufacturers achieve the 2 – 6 micron range. |
||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||
|
For connection systems such as Ankylos (4 degree conical) it is extremely difficult for laboratories to fabricate parts direct to implant (but they are starting to). Hence, the implants are usually fitted with manufacturers made abutments, which fit with a sub 2-micron microgap. |
||||||||||||||||||||||||||||||||||||
Conclusion |
||||||||||||||||||||||||||||||||||||
|
Restorative Dentists seldom specify to their technician what parts to use. Technicians like making prosthetics direct to implant head as it gives them more freedom and control. With some connection systems they can’t do this. With external hex, it is simple enough for them to achieve, what appears to be an acceptable fit to implant head. Most of these, including milled zirconia, have large microgaps. The solution is to use machined abutments, or if working direct to implant, to make use of the passive abutment system. |
||||||||||||||||||||||||||||||||||||
References |
||||||||||||||||||||||||||||||||||||
|
Byrne et al., Journal of Prosthetic Dentistry, 1998 Dellow et al., International Journal of Prosthodont, 1997 10:216 – 221 Kano et al., International Journal Oral Maxillofacial Implants, 2007 22:6 Tsuge et al., Dental Materials Journal, 2008 27:1 |
||||||||||||||||||||||||||||||||||||
|
By: G.A. Blackbeard (March 2011) |